Laser Surgery for Varicose Vein
At our centre all patients are treated with Latest Laser surgery.
Laser Proctology is now the standard care for Varicose Vein.
What are Varicose Veins?
Veins are the blood vessels of the body which carry impure blood to the heart. They carry blood towards the heart from the legs and hands and other parts of the body. The body’s natural movement helps pump blood back to the heart, which sends it out again through arteries in a continuous cycle.

All veins have valves that usually opens and closes to make sure blood is always flowing in the correct direction. Varicose veins are veins with broken valves. In a varicose vein, blood flows backward and stays in the vein. This causes the vein to expand, stretch, and become twisted, which prevents it from circulating blood effectively.
Varicose veins are typically affecting the superficial veins of the legs. Normally, superficial veins have one-way valves that help blood to flow back to the heart. If these valves become incompetent (open and non-functioning), blood pools in the veins causing them to become swollen and varicose. Sometimes varicose veins can also arise from structural weaknesses in the vein wall, or from higher than normal blood pressure in the veins.


Varicose veins are a common problem, affecting nearly 20- 30% of the population, with women more often affected than men by 2-3 times. The most common type of varicose veins is telangectasias. Due to their appearance, they may also be called spider veins, star bursts, thread veins, or matted veins.
Causes of Varicose veins:
- Older age
- Being female (hormonal changes from puberty, pregnancy, and menopause can lead to varicose veins, and taking birth control pills or hormone replacement can increase your risk)
- Being born with defective valves
- Obesity
- Pregnancy
- History of blood clots in your legs
- Standing or sitting for long periods of time
- Family history of varicose veins

Symptoms
Some patients experience no symptoms, but choose to see their doctor because they find the cosmetic appearance of varicose veins unsightly.
Symptomatic patients may experience:
- Dull ache or pressure in the legs after prolonged standing or walking
- Sensation of “heaviness” of the legs
- Skin changes (such as itchiness, pigmentation, induration)
- Recurrent or persistent ulceration
- Infection of the vein (phlebitis)
- Clots in the vein (thrombosis)
How are varicose veins diagnosed?
Usually Varicose veins are visible during a physical examination. Most of the patients need a duplex ultrasound to check the damage of the values. This test is a type of ultrasound that checks blood flow and the structure of the leg veins. Duplex means 2 kinds of ultrasound are used. With the help of this scan and the report, the appropriate treatment can be started.

How are varicose veins treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
If you don’t have symptoms, you may not need treatment. But varicose veins may sometimes get worse without treatment.
If you need treatment, it may include:
- Leg elevation. You may be instructed to raise (elevate) your feet above your heart 3 or 4 times a day for about 15 minutes at a time. If you need to sit or stand for a long time, bending (flexing) your legs now and then can help keep blood circulating. If you have mild to moderate varicose veins, elevating your legs can help reduce leg swelling and ease other symptoms.
- Compression stockings. These elastic stockings squeeze the veins and prevent blood from travelling down and pooling in the legs. They can be effective if they are worn every day from morning until night.
- Sclerotherapy. This is the most common treatment. A chemical is injected into the affected veins. The chemical causes scarring in the veins so that they can no longer carry blood. Blood then returns to the heart through other veins. The body absorbs the scarred veins.
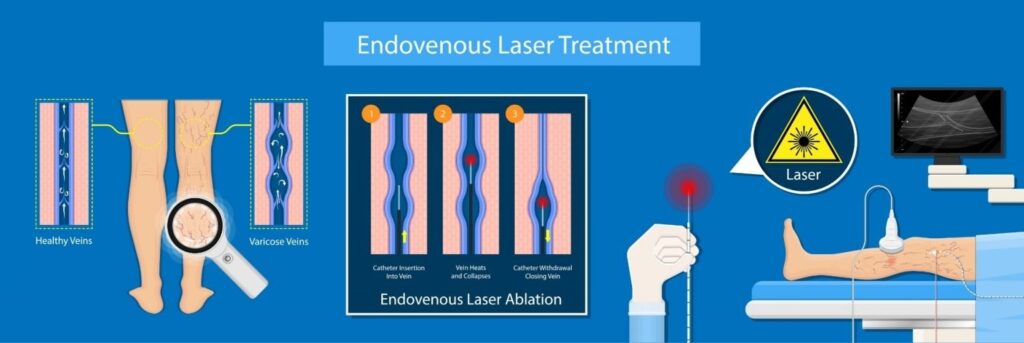
- Endovenous laser ablation or radiofrequency ablation (RFA). This is a minimally invasive procedure. A tube (catheter) puts heat right into the affected vein. This closes the vein. Once the vein is closed, less blood pools in the leg. Overall blood flow is improved.
- Vein stripping. In more severe cases or cases not suitable for laser treatment, the surgeon may tie off and remove veins by making small cuts in the skin. This procedure may be done when other treatments have not worked.But still, recurrence rates are always high

We at BariOSS Centre are treating the varicose veins with the most advanced laser and using the latest EVLA technology.
What is Endovenous Laser ablation for venous disease?
Endovenous laser ablation,is a newer technique that uses a laser or high-frequency radio waves to create intense local heat in the varicose vein or incompetent vein.
Heat is directed through a catheter to close up the targeted vessel. This treatment closes off the problem veins but leaves them in place so there is minimal bleeding and bruising.
Compared with ligation and stripping, many patients find that endovenous thermal ablation results in less pain and a faster return to normal activities, with similar cosmetic results.
Why is this procedure performed? Why do I need this procedure?
The goals of treatment are to reduce symptoms and reduce the risk of complications from venous disease, including blood clots.
Patients who have large, symptomatic varicose veins and those with incompetent saphenous veins are candidates for this procedure. This procedure is essentially taking the place of “vein stripping.”Each patient is evaluated, and treatment will be individualized for the patient’s circumstances.
How do I prepare for the procedure?
A few days before the procedure, pre-procedure tests may be performed to ensure that it is safe to perform the procedure. You may need to discontinue certain medications before the procedure. Our healthcare team will provide specific instructions to help you prepare for the procedure.
What happens during the procedure?
You will receive a sedative and a regional anaesthesia, or you may receive general anaesthesia as per the anaesthetist decision. Using an ultrasound to identify the location, our surgeon will insert a radial catheter and laser probe into the vein to be treated. This is typically done just below the knee, but can occasionally be done at the level of the ankle. Using ultrasound, the surgeon will inject a normal saline with soda bicarb solution and anaesthetic agent along the length of the vein to be treated. Following this, laser ablation will be performed.
How long does the procedure last?
The procedure itself generally takes one to two hours. This procedure is typically performed in the operation theatre. There may be a radiologist to assist locating the values for the surgeon and you can expect to be discharged home within 1 day after the procedure is complete. Full recovery will take approximately one to two weeks.

What happens after the procedure?
Our surgeon will give you specific instructions you need to follow after the surgery until your incision heals adequately. Typically, patients should elevate the treated limb when not moving, keep the incisions clean and dry, avoid swimming or hot tubs and wear compression bandages as prescribed.Compared with ligation and stripping, many patients find that endovenous thermal ablation results in less pain and a faster return to normal activities, with better cosmetic results
What are the risks and potential complications of the procedure?
Our surgeon will discuss the specific risks and potential benefits of the recommended procedure with you. This is generally a very safe procedure. However, as with any surgical procedure, there are risks. Complications after endovenous thermal ablation may include bruising along the site of ablation, pain along the site of ablation, the development of a blood clot in the veins in the treated leg, and irritation of the nerves that run along with the treated veins. Rarely, you may experience some numbness or tingling along the shin. These typically resolve over a couple of weeks.
Special precautions are taken to decrease these risks, and there may be other possible risks. When you consult without surgeon, please ask questions to make sure you understand the risks of the procedure and why the procedure is recommended.
Benefits of EVLA:
The biggest advantage for patients in opting for this type of varicose vein treatment is that it is non-surgical, with few potential complications. Other benefits include:
- Use of a spinal vs. a general anaesthetic
- Fast recovery period
- No significant scars
- Only minimal discomfort
- Low infection risk
- High rate of success
- Low rate of recurrence
- Excellent effectiveness over the long term
It is important for prospective patients to realize that no procedure to treat varicose veins will stop the formation of new blood vessels. For this reason, some patients return for additional treatments. Other common procedures to treat varicose veins are sclerotherapy and vein stripping.
What are the limitations of Endovenous Ablation of Varicose Veins?
Ablation catheters cannot easily pass through a vessel with many turns and bends. As a result, surgeons typically use ablation to treat superficial veins that lead to varicose veins. These may include the great saphenous vein, which extends from the groin and inside of the thigh to the ankle. Surgeons also commonly use ablation for other superficial veins, such as the small saphenous and accessory saphenous veins
Ablation is successful at closing the abnormal target vein almost 100 percent of the time, but small, dilated branches that persist in the skin often require additional treatment. These treatments may include phlebectomy or sclerotherapy.
What can I do to prevent varicose veins?
You may help prevent varicose veins by:
• Keeping a healthy weight
• Exercising regularly
• Putting your feet up while sitting
• Not crossing your legs while sitting
• Not wearing tight clothing
Do’s & Dont’s in Varicose Veins
DO:
- Maintain a normal weight.
- Avoid prolonged standing and sitting
- Regular exercise. Walking, swimming, or even chair exercises are great. Just move!
- Wear support stockings regularly. This increases blood in the legs back to the heart.
- Elevate your feet above your heart while sleeping. Elevate foot of bed using 2 or 3 pillows.
- Wear professionally made gradient support stockings that apply decreasing pressure on the leg from the ankle to knee.
- Watch carefully for folds in your support stockings. Knee length stocking should be just below the bend of the back of your knee by about 2 finger widths.
- Clip and file your toenails, to avoid snagging/running the stocking
- Stockings need to be washed after each wearing to maintain the shape and compression.
- Avoid activities that are likely to cause injury to legs or feet like walking barefoot.
- Wear support all day, and remove in the night during bed time.
- Make sure to wash your lower legs and feet regularly with mild soap and water.
- Be very careful if you shave your legs to avoid the thin walled veins that can be easily cut.
- Use moisturizing creams after washing legs;keep your legs clean and moisturized.
- Buy new stockings when you feel they are losingtheir support (feel less tight when you put themon).
- Get re-measured if your weight has changed bymore than 5 kgs.
- Wear support stockings during pregnancy.
DON’T:
Wear ACE bandages. Ace wraps do not provide proper compression.
Wear tight girdles, pants, boots, or any leg coverings that have tight tops that might have a tourniquet effect.
- Cross your legs.
Get measured for support stockings late in the day.
Wear jewelry when donning compressionstocking.
Walk around without footwear to protect thestocking.
Put on socks or leggings on first then cover itwith the compression stocking.
Wear your stockings to bed at night.
Fold the top of the stockings over.

Dr.Christopher S K
- bariosscentre@gmail.com
- 7708803335
- Bangalore, Chennai, Madurai, Tirunelveli, Nagercoil, Tuticorin, Tenkasi
FREQUENTLY ASKED QUESTIONS
A varicose vein is an enlarged, twisted vein, usually occurring in the leg. The formation of a varicose vein is caused by an obstruction within the vein, which causes it to swell. Varicose veins become visible and may bulge, and tiny capillaries can overfill, causing purple discoloration. Varicose veins can occur anywhere on the leg but are often found behind the knee or in the groin. There is often an inherited tendency to varicose veins and twice as many women as men tend to be affected. They can appear at any time but become more frequent with age.
The problems caused by varicose veins are not purely cosmetic although they are often unsightly. They can cause pain and discomfort and may itch. They can also cause a burning or throbbing sensation. After long periods of standing, swelling may occur. Sometimes in more severe cases, a vein can become inflamed (thrombophlebitis) or bleeding from a superficial vein (a vein near the surface of the skin) may occur.
Leg veins contain one-way valves that aid the return of blood to the heart. If there is increased resistance to blood flow in the leg because of pressure, the valves can become damaged and leaking may occur. Any leaked blood flows in the wrong direction, that is away from the heart and back down the leg, and causes the superficial veins to stretch and bulge. There tends to be an inherited predisposition to developing varicose veins although other factors may influence whether or not they actually develop. Increase in age may be a risk factor because, as you age, your veins may decrease in elasticity causing them to stretch. Occupations that require people to stand for prolonged periods of time (e.g., hairdressing, nursing) put people at greater risk of developing varicose veins if they have a genetic predisposition. Pregnancy can often cause varicose veins, but in most cases, these are temporary and will disappear a few months after the baby is born. Being very overweight puts increased pressure on the legs and can increase the likelihood of developing varicose veins.
Compression stockings can be used to alleviate many of the symptoms of varicose veins and can be useful for people in whom surgery is not advisable, for example, pregnant women. They may also be used to relieve symptoms and to prevent further damage in people whose veins are not severely affected. The stockings work by exerting pressure on the superficial veins to force blood into the deep veins of the leg and then back to the heart. They stop the blood from pooling and relieve the swelling of the veins. There are three different grades of stockings: light, medium and strong support. The appropriate grade should be chosen according to the severity of the problem. They are available in different sizes and colors and are prescribed by the surgeon to ensure that the correct degree of support is chosen and that they fit correctly.
Sometimes varicose veins may be treated with sclerotherapy. This treatment involves injecting the affected vein with a sclerosing agent which damages the lining of the vein. The walls of the vein then stick together and the vein will remain empty of blood. Treatment is not always permanent as the damaged valves are not repaired or removed so other veins can become affected. Larger varicose veins tend to be recurrent and sclerotherapy may only be a short-term measure. This method is often used as more of a cosmetic treatment for smaller capillaries, which are causing discoloration of the legs.
The usual treatment for severe varicose veins is surgery. Leaking valves, particularly those behind the knee or in the groin, may be removed. Alternatively, long stretches of veins can be stripped if they contain faulty valves. This is usually done via an incision in the groin and further small incisions down the leg. Large swollen varicose veins may also be tied off and removed. As it is only the superficial veins that become varicose, the main drainage of blood from the leg via the deep veins is unaffected by these procedures. The leg contains a complex of superficial and deep veins and blood will find another route back after veins have been removed. Faulty valves need to be removed or these new routes may also become varicose in time.
Latest Endovenous laser ablation can often be performed as day surgery although in some cases an overnight stay may be advised. Following EVLA most people are able to return to work or carry out normal activities after about 2 days (compared to patient who undergo open surgery where they need rest for 2 weeks).
Varicose veins may not be prevented but certain measures may be taken in order to reduce your risk of developing varicose veins or getting additional ones. Exercising, watching your weight, elevating your legs, and changing your sitting or standing position regularly have been shown to be helpful; these may also help treat the discomfort you may experience.
